Transforming Cities to Preserve the Health of Present and Future Generations
* This article was originally published by Santé publique France in La Santé en Action on December 15, 2022. Read the full issue dedicated to urban planning and health.
* One of the co-authors, Mathilde Pascale, is a Santé publique France representative in the IANPHI Committee on Climate Change and Health.

© City of Grenoble
According to the Intergovernmental Panel on Climate Change (IPCC), acting against climate change while protecting nature is essential to ensure a viable future. Urban areas, where 55% of the world’s population lives, are particularly vulnerable to climatic (extreme events, systemic crisis) and environmental (air pollution, heat waves, noise) risks. Faced with this situation, there is no inevitability: adapting urban environments to new climate challenges, reducing road traffic, encouraging active mobility such as walking or cycling and developing green spaces are all accessible and effective climate, biodiversity and public health‑friendly strategies. These initiatives represent major action points for local authorities, but strong determination in terms of intersectoral collaboration is required in order to achieve real transformation within cities.
At the end of 2021, on the sidelines of COP26, an international alliance of non-governmental organizations representing healthcare professionals from all over the world prescribed climate action as “a remedy for patients” [1]. A symbolic way of emphasizing that climate change is already claiming victims everywhere in the world, and that policies aimed at reducing greenhouse gas emissions and building adaptive capacities are essential to preserve health in all its dimensions, including mental health. The opinion of caregivers is consistent with that of researchers [2; 3] and public health agencies: climate action is public health action [4].
Unprecedented challenges
All of these communities agree on the need to act quickly, in a concerted and interdisciplinary manner. The unprecedented environmental, health and social challenges we face can no longer be addressed separately or on an ad hoc basis. The interdependence between the environment and health is now widely recognized, especially through the concepts of Planetary Health1 [5] and One Health2 [6]. The implementation of integrated preservation actions is essential [7]. According to the Intergovernmental Panel on Climate Change (IPCC), climate change mitigation, adaptation, nature conservation and the reduction of inequalities are essential for a “viable future” [7].
In terms of environmental challenges, climate change associated with the destruction of biodiversity and the alteration (in quality and quantity) of natural resources constitute a unique situation in human history. The planetary boundary theory was developed to help grasp the extent of environmental issues: it assesses the state of nine natural processes considered essential to the stability of the biosphere [8]. Five of these nine3 processes are already in a state of imbalance that threatens the terrestrial ecosystem: climate change; loss of biodiversity; changes in land use; disruption of global phosphorus and nitrogen bio-geochemical cycles4; chemical pollution [9]. Thus, it is insufficient to act solely on the climate, for example by investing in future technological solutions for trapping greenhouse gases. Societies need systemic transformation to redress these five imbalances that are already having massive impacts. Outdoor air pollution alone is responsible for 4.2 million premature deaths per year worldwide [10], including 40,000 deaths in mainland France [11].
We do not yet have indicators to globally quantify the effects of other planetary imbalances on health, but the IPCC already points to the dramatic impacts of climate change and its repercussions on natural and human ecosystems [7], via extreme climatic events, deterioration in the quantity and quality of food and water resources, mental health, certain infectious pathologies, or even migration. The World Health Organization (WHO) estimates that the health impacts are set to cost US$2–4-billion per year by 2030. This is a minimum estimate that only takes into account a small number of impacts [12].
Faced with this sombre observation, hope comes from the fact that it is possible to transform lifestyles and environments to simultaneously meet environmental, health and social challenges [5; 13]. This means mobilising new, creative and experimental approaches to tackle complex problems and help accelerate change, especially at city level [14].
Acting on the urban environment to protect the health of humans and ecosystems
Urban territories are among the places targeted for action to carry out these transformations. In 2018, approximately 55% of the world’s population lived in urban areas, a proportion that is expected to increase to 68% by 2050 [15]. These territories are also where the majority of economic wealth is concentrated [16]. Considered as complex socio-ecological systems, urban territories must be apprehended by adopting systemic approaches. However, the use of this type of approach and the importance of the repercussions in terms of health are still insufficiently considered by decision-makers [17].

Photo credit: J. Falguière
Urban territories are now very sensitive to environmental issues
Climate change increases the risk of complex crises via extreme events that lead to massive disorganization within urban systems [7]. These events can have lasting impacts on mortality, health care utilization or mental health.
In these territories, populations are overexposed to major health risks. Four out of the nine5 main environmental determinants of health [18] are omnipresent in urban areas: air pollution; temperature; noise; urban characteristics (urban fabric, built environment, land use, chemical pollution, etc.). However, these exposures are directly linked to the city’s organizational choices, particularly in terms of development, urban sprawl and transport, which also contribute to climate change. By acting on these choices, it is therefore possible to work both in favour of the environment and health, and to protect the health of current and future populations. This is, for example, the case of interventions aimed at reducing motorized mobility in favour of active mobility (i.e. non-motorized mobility, such as walking or cycling), which helps to reduce greenhouse gas emissions, while generating very significant health benefits [19] via increasing physical activity and reducing exposure to noise and air pollutants from road traffic.
To illustrate the importance of overexposure in urban areas, and therefore the potential co-benefits of interventions, we can note the considerable impact of environmental pollution generated by motorized mobility, which is the main form of transport today. Chronic exposure to ambient air pollutants is associated with the development of many diseases such as respiratory, cardiovascular and neurodegenerative diseases, perinatal health problems, and cancers. Air pollution is the first environmental determinant of health, with a considerable impact on quality of life, life expectancy and the health system. In France, almost three-quarters of deaths due to air pollution occur in urban communities (> 2,000 inhabitants) [20]. Noise, particularly related to traffic, is associated with one of the highest environmental disease burdens in Europe, after air pollution [21], mainly via the consequences of the discomfort caused, sleep disturbances and ischemic heart disease. It is also associated with learning disabilities in children.
Another example is how the lack of nature in the city aggravates exposure to heat. The latter is associated with the deterioration of many conditions such as mental health, cardiovascular, respiratory and renal diseases, and pre- or post-natal pregnancy-related pathologies affecting both mother and infant. The risk is exacerbated by the effects of urban heat islands (UHI) [22]. Heat waves are the deadliest extreme weather event in France today, totalling more than 39,500 deaths since 19746. The IPCC considers heat as one of the most important structural risks that Europe will face in the coming years [7].
In addition to their cooling effect on cities, green spaces are associated with an improvement in the overall state of health, mental health and even the behavioural development of children [23]. They also lead to a decrease in all-cause mortality [24; 25]. Be analysing different conceptual frameworks that illustrate how urban green spaces can contribute to health [26; 30], it is possible to assess the health potential of green spaces according to four main functions (see figure below). Although all of the mechanisms that could explain these benefits have not yet been fully elucidated, the conceptual frameworks proposed and the results of epidemiological studies are sufficiently robust to consider that lack of green space is one of the factors influencing mortality [31]. Urban green spaces thus represent major potential as a community intervention that simultaneously addresses public health issues (in particular the reduction of chronic diseases and their associated symptoms) and challenges linked to serious environmental changes, i.e. the fight against the effects of climate change and the protection of water resources and biodiversity [32; 33]. Thus, their implementation at all levels of urban land development has been strongly encouraged in recent years, as proved by the growing availability of documents supporting such action [34; 35].
Finally, there is a notable scarcity of scientific studies focusing on the health effects of biodiversity within cities (diversity of living species, wild fauna and flora). Also, the majority of existing studies analyse the risks (e.g. allergenics, stinging species, risks of zoonoses) and not the benefits. Some studies, however, point to co-benefits for mental health through actions that protect wildlife in the city [36]. Yet the deterioration of mental health is also one of the major impacts highlighted by the IPCC [7], as associated with extreme events but also with increasing anxiety about current environmental changes.
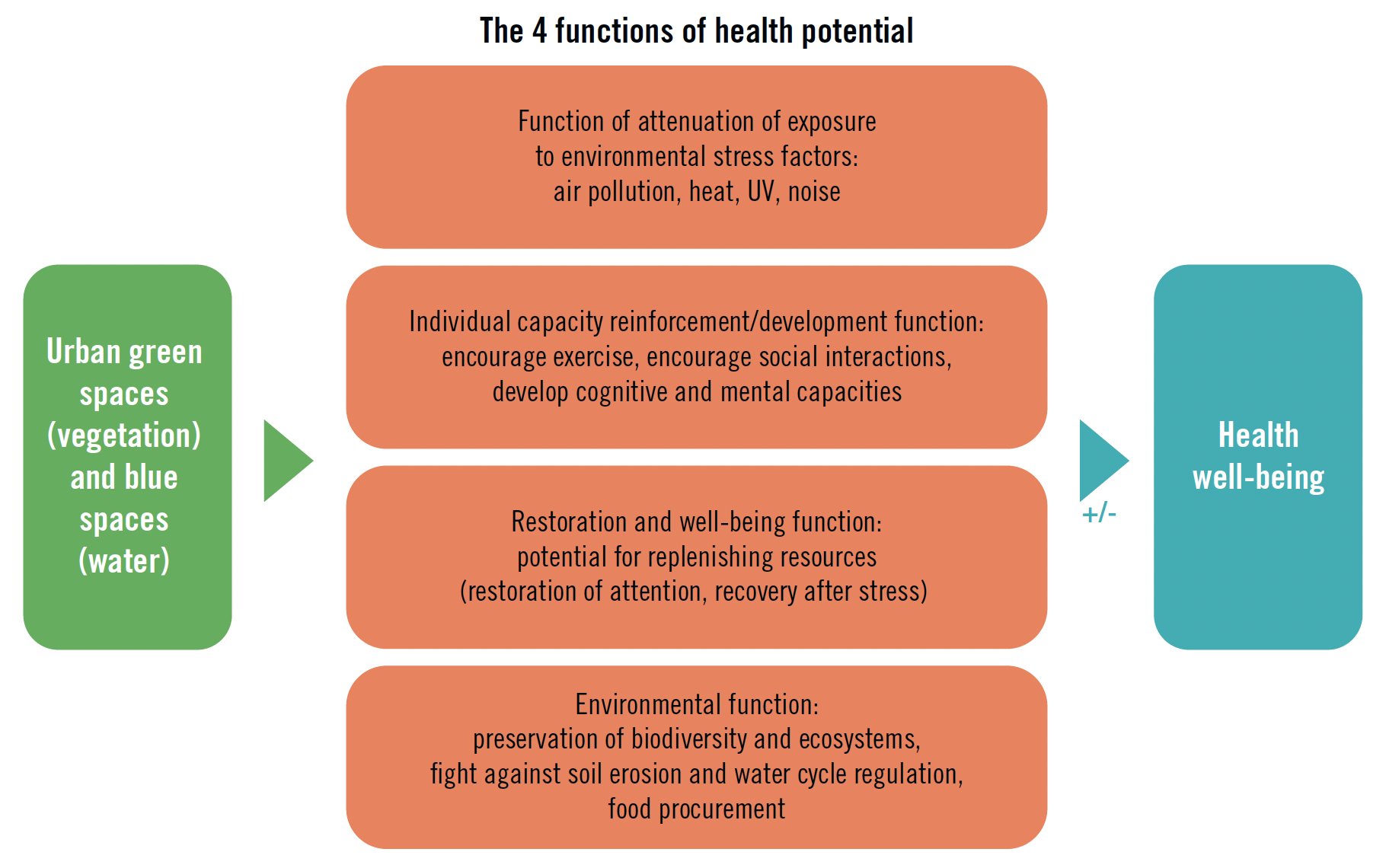
Figure. Effects of Green Spaces on Health [37]
Outlook
There is no turnkey solution to the current challenges, but there are many opportunities for action favourable to health, climate and biodiversity.
For researchers, it is a matter of supporting these developments via the dissemination of knowledge; through the co-production of tools adapted to the evaluation of these interdependent issues and decision-making; by the construction of productive interactions between scientists, decision-makers and society. The objective must be to better consider knowledge, as applied to a specific context, for decision-making [38]. These activities, called “boundary spanning”, go far beyond a simple process of disseminating science (via communication, applied science and advocacy).
For elected officials and municipal engineering services, as for other stakeholders in regional planning, priority should be given to setting up decision-making organizations and processes that tackle climate change adaptation and mitigation issues, protection of biodiversity and public health in a concerted manner. They must propose creative and evidence-based solutions that are adapted to the local context. This is all the more important since, in terms of healthy urban planning, adaptation and mitigation of climate change, and preservation of biodiversity, the several regulatory tools that exist too often operate in a disconnected way. The concept of health within all WHO policies aims to promote and facilitate inclusive and collaborative approaches [39] (see article “Urban health challenges: WHO findings and proposals” in the full issue of La Santé en Action).
——————
- Planetary Health integrates the health of human civilizations and the ecosystems on which it depends, in a cross-disciplinary approach.
- One Health is an integrated and unifying approach that aims to sustainably balance and optimize the health of people, animals and ecosystems.
- Other processes studied are ocean acidification, stratospheric ozone depletion, global freshwater use and aerosol loading.
- Transport and transformation of a chemical element between the atmosphere, the hydrosphere, the geosphere and the biosphere.
- The five other environmental determinants of health proposed by Rojas-Rueda et al. (2021) are environmental tobacco smoke, radon, heavy metals, radiation and chemical pollutants.
- Departmental data available on Géodes.santepubliquefrance.fr, Health determinants/Climate/Heat wave section
—————
For more information
Seminar dedicated to climate change and public health. Organized by Santé Publique France and the International Association of National Public Health Institutes.
——————
REFERENCES
[1] The Global Climate and Health Alliance. #ClimatePrescription Video: Why world leaders must take climate action to protect our health. 09 November 2021.
[2] Atwoli L., Baqui A. H., Benfield T., Bosurgi R., Godlee F., Hancocks S. et al. Call for emergency action to limit global temperature increases, restore biodiversity, and protect health. The Lancet, 2021, vol. 398, no. 10304: p. 939–941.
[3] Romanello M., McGushin A., Di Napoli C., Drummond P., Hughes N., Jamart L. et al. The 2021 report of The Lancet countdown on health and climate change: code red for a healthy future. The Lancet, 2021, vol. 398, no. 10311: p. 1619–1662.
[4] Pascal M., IANPHI roadmap for action on health and climate change engaging and supporting National Public Health Institutes as key climate actors. [Technical report] IANPHI, Novembre 2021: 8 p.
[5] Whitmee S., Haines A., Beyrer C., Boltz F., Capon A. G., Ferreira de Souza Dias B. et al. Safeguarding human health in the Anthropocene epoch: report of The Rockefeller Foundation – Lancet Commission on planetary health. The Lancet, 2015, vol. 386, no. 10007: p. 1973–2028.
[6] World Health Organization. Tripartite and UNEP support OHHLEP’s definition of “One Health”. [Press release] WHO, 1st December 2021.
[7] Pörtner H. O. Roberts D. C., Adams H., Adler C., Aldunce P., Ali E. et al. Climate Change 2022: Impacts, Adaptation, and Vulnerability. Working Group II contribution to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change. [Technical Summary] New York: Cambridge University Press, 2022.
[8] Rockström J., Steffen W., Noone K., Persson A., Chapin F. S., Lambin E. et al. Planetary boundaries: Exploring the safe operating space for humanity. Ecology and Society, 2009, vol. 14, no. 2.
[9] Persson L., Carney Almroth B. M., Collins C. D., Cornell S., de Wit C. A., Diamond M. L. et al. Outside the safe operating space of the planetary boundary for novel entities. Environmental Science & Technology, 2022, vol. 56: p. 1510–1521.
[10] World Health Organization. Ambient (outdoor) air pollution data 2022. September 2021.
[11] Medina S., Adélaïde L., Wagner V., de Crouy Chanel P., Real E., Augustin C. et al. Impact de pollution de l’air ambiant sur la mortalité en France métropolitaine. Réduction en lien avec le confinement du printemps 2020 et nouvelles données sur le poids total pour la période 2016-2019. Saint-Maurice: Santé publique France, coll. Studies and surveys, 2021: 64 p.
[12] World Health Organization. Climate change and health 2021. 30 October 2021.
[13] Intergovernmental Panel on Climate Change (IPCC). Global Warming of 1.5°C. An IPCC Special Report on the impacts of global warming of 1.5°C above pre-industrial levels and related global greenhouse gas emission pathways, in the context of strengthening the global response to the threat of climate change, sustainable development, and efforts to eradicate poverty. 2018.
[14] Grant M., Brown C., Calaffa W. T., Capon A., Corburn J., Coutts C. et al. Cities and health: an evolving global conversation. Cities & Health, 2017, vol. 1, no. 1: p. 1–9.
[15] United Nations. World urbanization prospects: The 2018 revision. [Press Release] New York, USA: United Nations Department of Economic and Social Affairs, Population Division, 2019.
[16] Rosenzweig C., Solecki W., Romero-Lankao P., Mehrotra S., Dhakal S., Bowman T. et al. Climate change and cities: second assessment report of the urban climate change research network. New York: Cambridge University Press, 2018.
[17] Chapman R., Howden-Chapman P., Capon A. Understanding the systemic nature of cities to improve health and climate change mitigation. Environment international, 2016, vol. 94: p. 380–387.
[18] Rojas-Rueda D., Morales-Zamora E., Alsufyani W. A., Herbst C.H., AlBalawi S. M., Alsukait R. et al. Environmental risk factors and health: An umbrella review of meta-analyses. International Journal of Environmental Research and Public Health, 2021, vol. 18, no. 2: p. 1–38.
[19] Nieuwenhuijsen M. J. Urban and transport planning pathways to carbon neutral, liveable and healthy cities; A review of the current evidence. Environment International, 2020, no. 140.
[20] Pascal M., de Crouy Chanel P., Corso M., Medina S., Wagner V., Goria S. et al. Impacts de l’exposition chronique aux particules fines sur la mortalité en France continentale et analyse des gains en santé de plusieurs scénarios de réduction de la pollution atmosphérique. Saint-Maurice: Santé publique France, 2016: 158 p.
[21] Hänninen O., Knol A. B., Jantunen M., Lim T.-A., Conrad A., Rappolder M. et al. Environmental burden of disease in Europe: assessing nine risk factors in six countries. Environmental Health Perspectives, 2014, vol. 122, no. 5: p. 439–446.
[22] Laaidi K., Zeghnoun A., Dousset B., Bretin P., Vandentorren S., Giraudet E. et al. The impact of heat islands on mortality in Paris during the August 2003 heat wave. Environmental Health Perspectives, 2012, vol. 120, no. 2: p. 254–259.
[23] World Health Organization, Regional Office Europe. Urban green spaces and health: A review of evidence, 2016.
[24] Rojas-Rueda D., Nieuwenhuijsen M. J., Gascon M., Perez-Leon D., Mudu P. Green spaces and mortality: A systematic review and meta-analysis of cohort studies. The Lancet Planet Health, 2019, vol. 3, no. 11: e469–e477.
[25] Twohig-Bennett C., Jones A. The health benefits of the great outdoors: A systematic review and meta-analysis of greenspace exposure and health outcomes. Environmental Research, 2018, vol. 166: p. 628–637.
[26] Lachowycz K., Jones A. P. Towards a better understanding of the relationship between greenspace and health: Development of a theoretical framework. Landscape and Urban Planning, 2013, vol. 118: p. 62–69.
[27] Hartig T., Mitchell R., de Vries S., Frumkin H. Nature and Health. Annual Review of Public Health, 2014, vol. 35: p. 207–228.
[28] Kuo M. How might contact with nature promote human health? Promising mechanisms and a possible central pathway. Frontiers in Psychology, 2015, vol. 6, no. 1093.
[29] Milvoy A., Roué-Le Gall A. Aménager des espaces de jeux favorables à la santé. La Santé en action, 2015, no. 434: p. 38–39.
[30] Markevych I., Schoierer J., Hartig T., Chudnovsky A., Hystad P., Dzhambov A. M. et al. Exploring pathways linking greenspace to health: Theoretical and methodological guidance. Environmental Research, 2017, vol. 158: p. 301–317.
[31] Bertrand C., Pascal M., Médina S. Do we know enough to quantify the impact of urban green spaces on mortality? An analysis of the current knowledge. Public Health, 2021, vol. 200: p. 91–98.
[32] Kingsley M. Climate change, health and green space co-benefits. Health Promotion and Chronic Disease Prevention in Canada, 2019, vol. 39, no. 4.
[33] Hunter R. F., Cleland C., Cleary A., Droomers M., Wheeler B. W., Sinnett D. et al. Environmental, health, wellbeing, social and equity effects of urban green space interventions: A meta-narrative evidence synthesis. Environment International. 2019, vol. 130.
[34] Roué Le Gall A., Thomas M.-F., Deloly C., Romagon J., Clément B., Nassiet C. Fiche Espace vert du guide ISadOrA (clef 12) Le guide ISadOrA, une démarche d’accompagnement à l’intégration de la santé dans les opérations d’aménagement urbain. EHESP, A-urba, FNAU, ADEME, DGS and DGALN, 2020: p. 249–280.
[35] Porcherie M., Roué-Le Gall A., Thomas M.-F., Faure E., Rican S., Vaillant Z. et al. Espaces verts urbains. Promouvoir l’équité et la santé. Rennes: French Network of Healthy Cities of the World Health Organization, 2020: 74 p.
[36] Aerts R., Honnay O., Van Nieuwenhuyse A. et al. Biodiversity and human health: Mechanisms and evidence of the positive health effects of diversity in nature and green spaces. British Medical Bulletin, 2018, vol. 127, no. 1: p. 5–22.
[37] Roué-Le Gall A. et al. Des espaces verts urbains favorables à la santé: De la théorie à l’action. In: Questionner l’évaluation : pour des stratégies et des actions favorables à la nature en ville. Plante & Cité, 2019, vol. 5: p. 32.
[38] Bednarek A. T., Wyborn C., Cvitanovic C., Meyer R., Colvin R. M., Addison P. et al. Boundary spanning at the science-policy interface: The practitioners’ perspectives. Sustainability Science, 2018, vol. 13, no. 1.
[39] Vallet B., Guilbert P. Prendre en compte la santé dans toutes les politiques publiques. La Santé en action, 2016, no. 435: p. 51–52.